How do organ donation and transplantation save lives? A critical examination of organ replacement procedures.
Organ replacement, a critical medical intervention, involves the surgical transfer of a biological component, like a kidney, heart, or lung, from a donor to a recipient. This process, often a last resort for patients with failing organs, restores functionality and improves quality of life. A successful procedure depends on meticulous surgical techniques, careful recipient evaluation, and robust immunosuppressant regimens to prevent rejection of the new organ.
The importance of this procedure is evident in the profound impact it has on the lives of recipients. Recovery from a successful transplant often leads to improved physical health and, in turn, greater independence and overall well-being. The historical development of transplantation, driven by advances in surgical techniques, immunology, and organ preservation methods, has significantly expanded the scope of this procedure and widened access to potentially life-saving treatment. The meticulous matching and compatibility considerations between donor and recipient, coupled with the necessity for long-term immunosuppression, highlight the complexity and precision required for successful transplantation efforts.
This discussion now shifts to explore the multifaceted challenges inherent in organ procurement, the ethical dilemmas surrounding donor selection and allocation, and the long-term management of transplant recipients. Furthermore, we will explore the latest advancements in this field, such as the innovative use of xenotransplantation and the ongoing quest for improved immunosuppressive therapies.
Clinical Transplant
Clinical transplantation, a complex medical intervention, hinges on meticulous planning and execution. Success relies on multiple interwoven factors, from donor compatibility to recipient health and immune response management. Understanding these aspects is crucial to appreciating the intricacies of this life-saving procedure.
- Organ viability
- Immunosuppression
- Recipient health
- Surgical skill
- Donor criteria
- Matching protocols
- Post-operative care
- Ethical considerations
Organ viability is paramount; a healthy donor organ is essential. Immunosuppression, vital for preventing rejection, necessitates careful monitoring. Recipient health, both physical and immunological, significantly impacts outcomes. Surgical skill is critical for successful transplantation. Donor selection criteria prioritize compatibility and health. Matching protocols ensure optimal organ compatibility. Post-operative care is crucial for managing complications and promoting healing. Ethical considerations play a vital role in the entire process. These factors interrelate; for instance, a poorly matched organ and inadequate immunosuppression increase rejection risk. Ultimately, the intricate interplay of these elements underscores the complexity and significance of clinical transplantation.
1. Organ Viability
Organ viability is a fundamental prerequisite for successful clinical transplantation. The health and functional capacity of the donated organ directly impact the likelihood of a positive outcome for the recipient. Maintaining organ viability during procurement, transport, and pre-transplant storage is crucial to preserving its structural integrity and cellular function. Compromised viability can lead to organ failure, rejection, and ultimately, negative consequences for the recipient.
- Donor Source and Preservation Techniques
The source of the organ significantly influences its viability. Organs sourced from deceased donors require rapid retrieval and preservation methods like cold storage with specific solutions to maintain viability during transport and storage. These methods aim to minimize ischemia time the period of oxygen deprivation to preserve cellular function. Optimal preservation techniques are crucial for maintaining organ viability and functionality until transplantation can occur. Examples include the use of specific cold storage solutions and specialized transport systems designed for organ preservation. Variations in preservation techniques and standards can significantly influence the success of clinical transplantation. Improper handling or extended ischemia time negatively impact organ viability.
- Assessment of Organ Function
Pre-transplant evaluation of the organ's function is essential. Tests assess the organ's structural integrity, the viability of its cells, and its ability to perform its intended physiological role. The presence of infections, diseases, or damage can compromise organ viability and increase the risk of complications after transplantation. Thorough screening protocols and detailed assessments aim to select organs with optimal viability for transplantation.
- Impact on Immunological Response
Organ viability directly affects the recipient's immunological response. A viable organ is less likely to be rejected because its cells retain their natural structure and functionality. Damage or cellular stress in the organ, however, can trigger an exaggerated immune response, leading to a higher chance of rejection.
- Impact on Long-Term Outcome
Organs with optimal viability tend to perform better in the recipient and are associated with better long-term outcomes. In contrast, those with suboptimal viability may not function optimally after transplant or have an increased risk of rejection, impacting the recipient's long-term health and survival. A direct link exists between the quality of the transplanted organ and the overall success and longevity of the transplantation procedure.
In conclusion, organ viability is a paramount consideration throughout the entire clinical transplantation process. Prioritizing and optimizing donor organ viability is critical to successful transplantation and maximizing long-term outcomes for recipients.
2. Immunosuppression
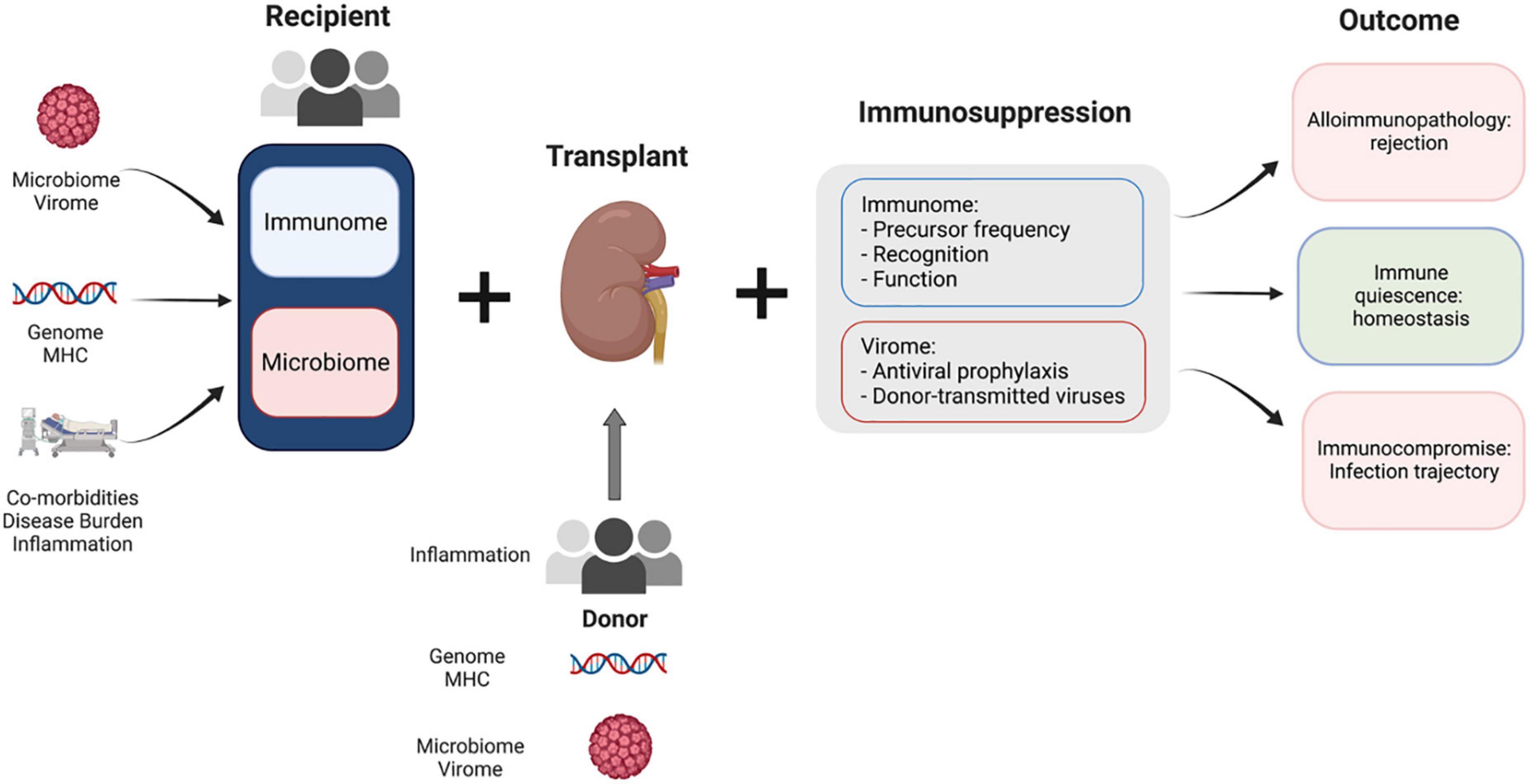
Immunosuppression plays a critical role in clinical transplantation. The transplanted organ, originating from a different individual, is recognized by the recipient's immune system as foreign tissue. This triggers an immune response designed to eliminate the perceived threat. Without intervention, the recipient's immune system would attack and reject the transplanted organ. Immunosuppressive therapies act to mitigate this immune response, preventing rejection and promoting the long-term survival of the grafted tissue.
The efficacy of immunosuppression is directly linked to the success of a clinical transplant. The strength and duration of immunosuppressive regimens are tailored to the individual recipient and the specific organ transplanted. Precise dosage and timing are crucial to minimize rejection while mitigating the potential for adverse effects associated with immunosuppression. Examples include chronic kidney disease patients receiving a kidney transplant who require lifelong immunosuppression to prevent the rejection of the new kidney, or heart transplant recipients who may have to carefully manage immunosuppressive drugs to prevent complications such as infections. This complex interplay underscores the importance of carefully monitoring recipients and adapting immunosuppressive strategies throughout the post-transplant period.
The significance of immunosuppression in clinical transplantation cannot be overstated. Maintaining a balance between preventing organ rejection and minimizing the risk of opportunistic infections or other adverse effects associated with prolonged immunosuppression requires ongoing vigilance and clinical expertise. This necessitates close collaboration between transplant surgeons, immunologists, and other healthcare professionals. Ongoing research in this area seeks to develop more effective and less toxic immunosuppressive agents, thereby improving outcomes and reducing the long-term health risks associated with clinical transplantation for recipients. Ultimately, a thorough understanding of immunosuppression is critical to maximizing the success and longevity of these life-saving procedures.
3. Recipient Health
Recipient health represents a critical determinant in the success or failure of clinical transplantation. Pre-existing medical conditions, immunological status, and overall physical well-being directly impact the recipient's ability to tolerate the procedure and the long-term survival of the transplanted organ. Assessment of these factors is paramount to risk stratification and optimal patient selection.
- Pre-existing Medical Conditions
Pre-existing conditions significantly influence the recipient's suitability for transplantation. Conditions such as cardiovascular disease, diabetes, or chronic respiratory illnesses can increase the risk of complications during and after the procedure, and negatively impact the long-term success of the transplant. Precise evaluation and management of these conditions prior to transplantation are essential. For example, controlling blood sugar levels in a patient with diabetes is crucial to reduce the risk of complications from the transplant surgery and maintain healthy organ function in the long-term.
- Immunological Status
The recipient's immunological status directly impacts the risk of organ rejection. Individuals with compromised immune systems, such as those with certain cancers or HIV, are at higher risk of organ rejection and may require adjusted immunosuppressive regimens or potentially preclude them from transplantation entirely. Factors impacting immunological status must be evaluated carefully and considered in the recipient selection process. For instance, a patient with uncontrolled autoimmune disease may experience heightened risk of rejection post-transplant.
- Overall Physical Well-being
General physical condition, including nutritional status and overall health, plays a substantial role in the recipient's ability to recover from the procedure. Poor nutrition or existing weight issues can significantly impact recovery and increase the risk of complications. For example, malnourished patients may have a harder time recovering from the surgical procedure and are more susceptible to infections, potentially endangering both the transplanted organ and the recipient's health.
- Age and Other Factors
Age and other factors such as genetics, smoking history, and alcohol use also influence the recipient's ability to tolerate the procedure and immunosuppression. Elderly individuals often present more complex cases than younger ones. These age-related factors, along with pre-existing medical conditions, must be carefully considered for appropriate patient selection. This process often necessitates individualized assessment and treatment plans to optimize patient outcomes.
In summary, recipient health encompasses a wide range of factors that significantly impact the success of a clinical transplant. Thorough evaluation, comprehensive pre-transplant assessments, and ongoing management of health conditions are crucial to reduce risks and improve patient outcomes. Furthermore, the individual variations in recipient health necessitate individualized treatment approaches tailored to each patient to optimize post-transplant care.
4. Surgical Skill
Surgical skill is inextricably linked to the success of clinical transplantation. Precise and delicate manipulation of tissues is essential to minimize trauma to both the donor organ and the recipient's anatomy. Surgical technique profoundly influences the safety and efficacy of the procedure. Minimizing tissue damage during organ procurement and transplantation reduces the risk of complications, such as bleeding, infection, and organ dysfunction. A surgeon's experience and proficiency directly impact the preservation of organ viability. Skilled surgeons meticulously coordinate procedures to ensure optimal blood flow and minimize damage to surrounding tissues.
Errors in surgical technique, such as improper suturing or excessive tissue manipulation, can lead to complications, potentially compromising the survival of the transplanted organ. This underscores the importance of surgeons possessing the technical expertise to perform intricate procedures with precision. Experience in complex vascular anastomosis, crucial for connecting blood vessels, is essential for successful organ transplantation. Examples include the precise re-establishment of blood flow in heart-lung transplants or the creation of delicate anastomoses in kidney or liver transplants. The meticulous nature of these procedures demands a high level of expertise and proficiency, influencing the long-term health of the recipient. This expertise is vital to preventing complications such as bleeding, thrombosis, or organ rejection.
Proficiency in surgical technique is critical for optimal patient outcomes in clinical transplantation. A skilled surgeon's ability to execute the procedure with precision and minimal invasiveness greatly reduces the risk of post-operative complications and enhances the long-term survival of the transplanted organ. This underscores the importance of ongoing training, advanced surgical techniques, and the emphasis on maintaining surgical proficiency within the field of transplantation. Understanding this profound correlation between surgical skill and clinical transplantation is vital for fostering a culture of excellence and improving patient outcomes.
5. Donor Criteria
Donor criteria in clinical transplantation are meticulously defined and rigorously applied. These criteria directly impact the safety and efficacy of the transplantation process, and are crucial for selecting donors whose organs are most compatible and viable. Meeting these stringent criteria is essential for ensuring the best possible outcome for the recipient.
- Compatibility Matching
Matching donor organs to recipient tissues is paramount. Blood type compatibility is a fundamental requirement. Beyond this, tissue typing, focusing on human leukocyte antigens (HLAs), ensures minimal likelihood of rejection. In essence, the closer the match, the lower the risk of immune system rejection post-transplant. Mismatches increase the need for strong immunosuppressants and the risk of rejection episodes, potentially compromising the success of the transplant. Precise tissue matching is a critical process that directly relates to the longevity and health of the recipient post-transplant.
- Organ Viability and Health
Organs must meet stringent viability standards. Factors like the time since death, the presence of any underlying diseases or damage (such as infection or trauma), and blood flow during procurement and transport directly influence organ viability. Organs exhibiting signs of deterioration or damage are often unsuitable for transplantation, potentially compromising recipient health. Determining the ideal window for organ retrieval is crucial for maximizing organ survival post-transplantation. The quality of the organ procured is paramount to the overall success of the transplant.
- Donor Health Status
Donors, whether deceased or living, must be screened for pre-existing medical conditions that might compromise organ function or increase the risk of complications. Certain infections, or chronic diseases like uncontrolled hypertension or diabetes, are unacceptable. The donor's history and physical condition are carefully considered to ensure the viability and safety of the donated organ. Factors like smoking or alcohol abuse might also be excluded factors. Screening for these conditions ensures the safety of both the donor and the recipient, potentially impacting the overall success of the transplant.
- Ethical Considerations
Ethical frameworks underpin donor selection. Donor families' informed consent and the transparency of the process are integral components. Protocols and regulations are designed to ensure that the procedure is conducted in compliance with ethical guidelines. These guidelines prioritize the well-being of both the donor and the recipient. These ethical considerations prevent exploitation and guarantee a just and fair process in organ allocation.
In summary, donor criteria are essential to the entire process of clinical transplantation. Strict adherence to these criteria is not merely a formality; it directly translates to the recipient's health and the long-term success of the transplant. Careful evaluation, adherence to ethical standards, and robust screening are essential to ensuring the highest possible standards of care throughout the process.
6. Matching protocols
Matching protocols are fundamental to the success of clinical transplantation. These protocols dictate the selection process for donor organs, ensuring compatibility with recipient tissues. Accurate matching minimizes the risk of rejection, a critical factor in achieving long-term graft survival. Precise identification of compatible tissues is a cornerstone of successful transplantation.
- HLA Matching
Human Leukocyte Antigen (HLA) matching is central to transplant compatibility. HLA molecules are cell surface proteins, and their diversity dictates an individual's immune response. Matching donors and recipients with similar HLA profiles significantly reduces the likelihood of immune-mediated rejection. The degree of HLA matching influences the strength and duration of immunosuppression required post-transplant, impacting long-term health and reducing the risk of rejection episodes. Close HLA matching greatly improves the chances of successful graft integration and survival. Sophisticated algorithms and databases are used to identify the most compatible donors based on HLA profiles.
- Blood Group Matching
Blood group compatibility is a fundamental initial step. Incompatible blood groups can lead to severe complications, including hemolysis, and must be strictly adhered to. Mismatches can trigger potentially life-threatening reactions. Precise identification of blood groups before transplantation is essential to ensure a safe and effective procedure.
- Tissue Typing and Compatibility Criteria
Tissue typing extends beyond blood groups and HLA matching, incorporating factors like tissue structure and potential immunological sensitivities. Comprehensive tissue typing identifies genetic variations affecting cellular recognition and response. This nuanced analysis is essential for tailoring immunosuppressive strategies, reducing the chance of rejection, and ultimately improving patient outcomes. Different organs require varying degrees of tissue typing specificity. Liver transplants, for instance, demand detailed evaluations of histocompatibility for optimal outcomes. Sophisticated protocols ensure that recipient and donor tissue characteristics are rigorously examined and considered during the matching process.
- Donor Organ Assessment
Beyond matching, protocols include meticulous assessment of the donor organ's viability. This evaluation considers factors like preservation time, the extent of any damage or disease, and overall tissue quality. Compromised organs are unsuitable regardless of matching criteria, as they are unlikely to function effectively in a recipient's body. Quality controls and pre-transplant testing of donor organs reduce risks associated with transplantation.
In conclusion, matching protocols in clinical transplantation are more than just procedures; they are crucial steps in ensuring long-term graft success. These protocols integrate sophisticated scientific principles to optimize outcomes, minimizing rejection risk and improving the quality of life for recipients of organ transplants. Thoroughness in matching protocols is a testament to the dedication to safe and successful clinical transplantation procedures.
7. Post-operative care
Post-operative care is an indispensable component of clinical transplantation, directly influencing the success and long-term well-being of transplant recipients. The meticulous management of recipients post-surgery is crucial for preventing complications, mitigating rejection, and promoting successful engraftment of the transplanted organ. Post-transplant care involves a complex interplay of medical interventions aimed at supporting the recipient's physiological recovery and managing immune responses. Examples include the administration of immunosuppressive medications, vigilant monitoring for signs of rejection or infection, and the provision of comprehensive rehabilitation programs to maximize functional recovery.
The importance of post-operative care extends beyond immediate recovery. Early detection and intervention for complications, such as organ rejection or infections, are essential for maintaining long-term organ function. The success of a transplant hinges critically on adherence to rigorous post-operative protocols. These protocols encompass meticulous monitoring of vital signs, blood tests, and assessment of immunosuppressant drug levels. This detailed approach ensures that any potential issues are identified promptly, facilitating prompt and effective management. Real-life examples demonstrate that consistent adherence to post-operative protocols significantly correlates with better long-term outcomes. Patients who diligently adhere to prescribed medications and attend follow-up appointments experience lower rates of complications and prolonged graft survival. Conversely, inadequate or inconsistent post-operative care can lead to serious complications, potentially necessitating organ removal or negatively impacting the quality of life for the recipient.
In conclusion, post-operative care in clinical transplantation is not merely a set of procedures; it's a critical element of the entire process, profoundly influencing long-term outcomes. Comprehensive post-operative care, encompassing meticulous monitoring, appropriate medication management, and diligent follow-up, is crucial for optimizing graft survival and enhancing the overall health and well-being of transplant recipients. The implications extend beyond individual patient care, highlighting the importance of robust post-transplant support systems in healthcare facilities. Future advancements in monitoring technologies and targeted immunosuppressive therapies are likely to further refine post-operative care, leading to even better outcomes for transplant recipients.
8. Ethical Considerations
Ethical considerations are inextricably interwoven with clinical transplantation. The unique nature of this life-saving procedure raises complex moral dilemmas that must be addressed with careful scrutiny and a commitment to fairness and justice. These considerations encompass the allocation of scarce resources, the treatment of potential donors and recipients, and the potential for exploitation or coercion in the context of organ procurement and transplantation.
- Donor Selection and Allocation
The selection and allocation of organs for transplantation raises complex ethical dilemmas. Criteria for donor selection necessitate balancing the needs of potential recipients with the ethical imperative to ensure equitable access and avoid exploitation. Considerations include factors such as medical urgency, the likelihood of successful transplantation, and the potential for long-term health outcomes for both the donor and recipient. Transparency and fairness in these processes are crucial to maintain public trust and prevent the perception of favoritism or discrimination.
- Informed Consent and Autonomy
Informed consent is paramount in both deceased and living donor situations. Individuals or families must be fully informed about the risks and benefits associated with organ donation or transplantation. Respect for patient autonomy demands that these decisions be made freely, without coercion or undue influence. Issues arise when considering the potential for coercion or undue pressure, especially in marginalized communities or cultures where financial or social incentives could sway decisions. The preservation of informed consent guarantees a free and informed choice.
- Resource Allocation and Equity
Organ transplantation, as a complex and resource-intensive process, necessitates careful resource allocation. Competing demands for these vital resources necessitate clear and equitable guidelines to determine which patients receive the procedure. Ethical frameworks must ensure access is determined by clinical need, urgency, and potential for positive outcomes rather than socioeconomic status, or geographic location. The prioritization of certain recipients and allocation procedures require consistent and transparent guidelines to avoid bias and maintain equity.
- Potential for Exploitation and Commodification
The potential for exploitation and the commodification of human organs poses significant ethical challenges. The economic incentives and pressures surrounding organ donation could potentially lead to unfair practices or exploitation, particularly if vulnerable populations are targeted. Robust regulations and oversight are necessary to prevent exploitation and ensure that financial gain does not compromise ethical considerations. Measures to protect vulnerable populations and ensure fair treatment of all involved are essential for maintaining ethical standards.
These facets highlight the multifaceted nature of ethical considerations in clinical transplantation. The need for transparency, fairness, and equitable access are crucial for maintaining public trust and ensuring the integrity of this life-saving procedure. Ongoing dialogue and evolving ethical frameworks are essential to address the dynamic nature of these complex issues and promote the safe and responsible advancement of transplantation techniques.
Frequently Asked Questions About Clinical Transplantation
Clinical transplantation involves the surgical replacement of a diseased or damaged organ with a healthy one. This complex procedure raises numerous questions. This section addresses some frequently asked queries surrounding clinical transplantation.
Question 1: What are the eligibility criteria for organ transplantation?
Eligibility criteria vary depending on the organ being transplanted and the specific recipient's circumstances. Essential factors include the severity and nature of the recipient's organ failure, overall health status, medical history, and immunological profile. Compatibility matching with a suitable donor is another critical factor, often evaluated through blood type and tissue typing (HLA matching). The recipient's overall physical and mental health must allow for the rigors of the surgical procedure and subsequent post-transplant care. Patients must demonstrate the capacity to manage the long-term immunosuppression required to prevent organ rejection.
Question 2: What are the risks associated with organ transplantation?
Clinical transplantation, while life-saving, carries inherent risks. These include complications during the surgical procedure, such as bleeding and infection. Post-operative complications can arise, like organ rejection, where the recipient's immune system attacks the transplanted organ. Long-term risks involve the side effects of immunosuppressive medications, increasing susceptibility to infections and other complications. Careful monitoring and management are crucial to mitigate these potential risks.
Question 3: How is the donor organ sourced?
Donor organs are sourced from deceased or living donors. In the case of deceased donors, rigorous evaluation of organ viability, considering factors like time since death and potential diseases, is crucial. Living donors often undergo careful screening, including medical evaluations and immunological testing, to ensure their suitability and to minimize risk to their own health. Ethical considerations and legal frameworks govern the acquisition of organs from both deceased and living donors.
Question 4: How long does the recovery process typically take after a transplant?
Recovery time varies significantly depending on the specific transplant and the individual's response to the procedure. Initial recovery may require hospital stays of several weeks to manage immediate post-operative complications. Long-term recovery is a gradual process that can span several months or even years. Adherence to prescribed medications and regular follow-up appointments with healthcare providers are essential for successful long-term outcomes. The complexities of immunosuppression contribute to the length of the recovery period.
Question 5: What is the role of immunosuppression after transplantation?
Immunosuppression is crucial after transplantation to prevent the recipient's immune system from rejecting the new organ. This involves medication regimens designed to suppress the immune response to the transplanted tissue. However, this medication often has side effects and increases the risk of infections. The goal is to strike a balance between suppressing rejection and minimizing the risk of adverse effects. Maintaining the right medication levels and monitoring for complications are critical elements in post-transplant care.
These frequently asked questions highlight the complexities inherent in clinical transplantation. Careful consideration of pre-transplant factors, the inherent risks, and rigorous post-operative care are integral parts of the process. Ethical considerations related to allocation and informed consent further underline the multifaceted nature of organ transplantation.
This section concludes the FAQ section. The next section will delve into the latest advancements and breakthroughs in the field of transplantation.
Conclusion
Clinical transplantation, a complex and multifaceted medical intervention, necessitates meticulous planning, precise execution, and sustained post-operative care. This process, while offering hope to individuals with failing organs, demands a profound understanding of immunological principles, surgical expertise, and ethical considerations. The article explored key factors such as organ viability, the critical role of immunosuppression, the importance of recipient health, the precision of surgical technique, the necessity of careful donor selection and matching, the complexities of post-operative care, and the ethical frameworks that guide the procedure. These interconnected elements highlight the significant responsibility inherent in clinical transplantation.
The future of clinical transplantation hinges on continued advancements in organ preservation techniques, the development of novel immunosuppressive therapies with fewer side effects, and the refinement of matching protocols. Furthermore, addressing ethical dilemmas, ensuring equitable access, and mitigating the potential for exploitation are critical considerations. Clinical transplantation represents a significant medical triumph, but its continued success relies on ongoing research, careful ethical deliberations, and unwavering dedication to patient well-being. The field faces continuous challenges demanding persistent innovation and a commitment to responsible medical advancement.


Detail Author:
- Name : Dr. Douglas Kuhlman
- Username : egreen
- Email : lucas18@gmail.com
- Birthdate : 1997-04-26
- Address : 4971 Wanda Shore Apt. 527 West Stacy, MA 78549-8154
- Phone : 203-570-5182
- Company : Halvorson, Rogahn and Kshlerin
- Job : Electronics Engineer
- Bio : At eos eligendi rerum. Itaque unde quia hic sed aut. Non quis nobis natus minima.
Socials
instagram:
- url : https://instagram.com/wilma3009
- username : wilma3009
- bio : Ut eum adipisci molestias est quia. Dolorum omnis amet quod.
- followers : 6424
- following : 1215
facebook:
- url : https://facebook.com/prohaska2007
- username : prohaska2007
- bio : Non molestiae et deserunt sit dolor.
- followers : 3011
- following : 2758
tiktok:
- url : https://tiktok.com/@wilma_prohaska
- username : wilma_prohaska
- bio : Nesciunt sed labore perspiciatis dolore molestiae adipisci dolorem.
- followers : 4719
- following : 529
twitter:
- url : https://twitter.com/wilmaprohaska
- username : wilmaprohaska
- bio : Voluptatem neque esse officia corrupti ut beatae quia. Ipsa eaque perferendis molestiae consequuntur laborum. Vel aut error alias recusandae architecto.
- followers : 4709
- following : 18